CLINICAL STUDIES
Solutions Rooted in Clinical
Research Collaborations
Dedicated to improving the quality of life of patients with chronic conditions, we are committed to funding and collaborating on research that supports the advancement of free-living, consumer-friendly devices to monitor symptoms, disease progression and the development of personalized treatments.
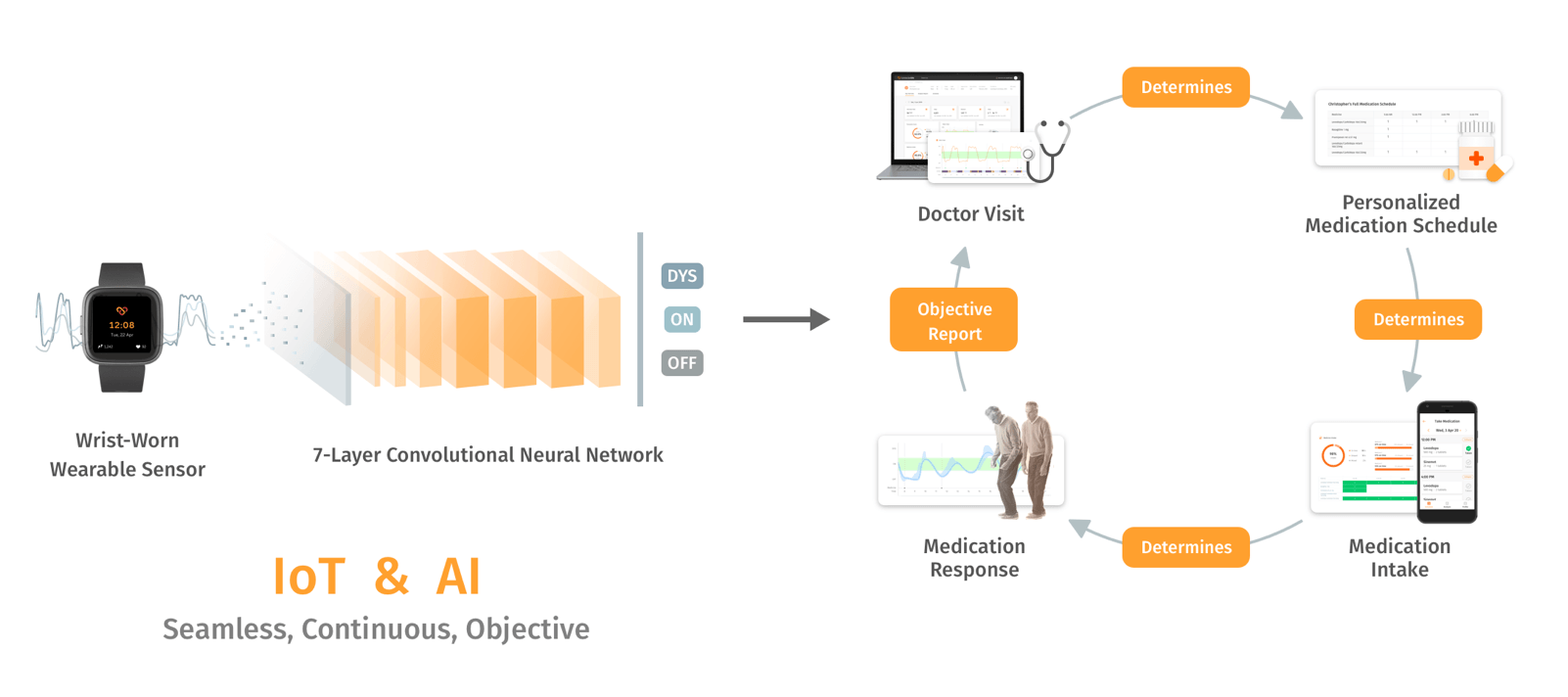
Closed loop technology (CLT) has the potential to innovate medical therapies. In order to implement monitoring of specific medical conditions into the daily lives of patients, CLT needs to (i) work seamlessly for the patient, (ii) provide a continuous readout on patient’s health conditions, and (iii) provide healthcare professionals with objective and reliable data. This is the core of what we do at ConnectedLife, in our consistent bid to improve the quality of life of people with chronic conditions, and to transform the patient-clinician care assessment.
We seek to validate our work in the fields of Parkinson’s Disease and Orthopaedics via observational work and classification by clinical experts, to ensure the accuracy of the outcomes. Our clinical trials currently in progress harden the implementation of the developed model, with an end-to-end product solution. We test the system with multiple wearable devices to achieve a generalised model.
Parkinson’s Disease
Inspired by our early work in Orthopaedic complications, we initiated exploratory work in Parkinson’s Disease in Germany. Franz MJ Pfister (2017 – 2019: Chief Medical Officer, ConnectedLife GmbH) and Kamer Ail Yuksel (2018 – 2019: Chief Data Scientist, ConnectedLife GmbH), undertook the following research theorizing the use of wearables and technology to continuously monitor Parkinson’s symptoms, in a similar way to Diabetes management. Devices were provided to Schön Klinik, with our biomedical data science team in Munich and University research collaboration partners focused on data collection and driving development and training of the Deep Learning algorithm. In Singapore, the data science team pre-processed the data, generated and labelled the input images, while the product development team focused on building the end-to-end platform for both patients, clinicians and administrators.
Below are details covering the ongoing clinical research collaboration with the National Neuroscience Institute Singapore (NNI, 2018 – 2022) and research papers undertaken for Parkinson’s Disease our colleagues and collaborators have published in recent years.
Monitoring Parkinson’s Disease (Ongoing from 2018)
National Neuroscience Institute of Singapore (CIRB Ref: 2018/2012)
- A clinical research collaboration using deep learning for data processing and data analytics, to validate that an objective measurement of the Parkinson’s Disease motor state and motor symptoms is possible with a single wrist-worn device.
- Sub-study groups of Deep Brain Stimulation (DBS) candidates versus non-DBS candidates with changing medication dose are included.
Wearable-based Parkinson’s Disease Severity Monitoring using Deep Learning
Goschenhofer J, Pfister FMJ, Yuksel KA, Bischl B, Fietzek UM, Thomas J
- Evaluation was done using a leave-one-patient-out validation strategy on 28 Patients with Parkinson’s using a customized performance measure, developed in cooperation with medical experts in the Parkinson’s Disease domain
- The deep learning approaches outperformed the classic machine learning approach and results suggest that deep learning techniques offer a high potential to autonomously detect motor states of patients with Parkinson’s disease
- More high-quality labelled data is required to further successfully train the model. This highlighted the need to run an extended clinical trial with the National Neuroscience Institute in Singapore where a further 100 patients could be added to the training model on top of testing an end-to-end solution
Granular Motor State Monitoring of Free-Living Parkinson’s Disease Patients via Deep Learning
Yuksel KA, Goschenhofer J, Varma HV, Fietzek U, Pfister FMJ
- This paper is an extension of a previous work within which performances of classification, ordinal classification and regression on the motor fluctuation estimation problem using state-of-art time series classification architectures were compared
- State-of-the-art architecture for the motor fluctuation estimation using a regression setting
- Pre-training technique for improving the generalization of the model to previously unseen patients while training with a limited clinically labelled dataset
- Relaxed loss function with the aim of tackling the discreteness noise by the labels given by clinical raters
- Experimental results showed that accurate estimation of nine-level motor fluctuation severity of Parkinson’s Disease patients, which is one of the most relevant constructs for the clinical decision-taking in Parkinson’s Disease, is possible in the comfort of their home
- This accurate estimation can enable optimizing the medication schedule and dose in such a way that the patient has an improved chance to spend the entirety of his waking day in normal state; in other words, achieving a stable ON condition while impeding OFF or dyskinetic motor states
- The personalized medication, which should be adapted as the disease progresses, can allow improving the life of Parkinson’s Disease patients who are suffering from severe symptoms, just because of the imperfect medication
A Multi-layer Gaussian Process for Motor Symptom Estimation in People with Parkinson’s Disease
Lang M, Pfister FMJ, Frö̈hner J, Abedinpour KP, Pichler DC, Fietzek UM, Um TT5, Kulić D, Endo S, Hirche S
- Multi-layered Gaussian Process model used estimates severity of different Parkinson’s Disease-related Movement abnormality classes:
- Tremor (Bradykinetic or dyskinetic)
- Non-tremulous Bradykinesia
- Non-tremulous Dyskinesia
- Focus on collection of unscripted motion data, thus Parkinson’s Disease estimation can take place during unconstrained free living activities
- Single commercially available wrist-worn low cost wearable sensor used to demonstrate robustness and applicability of approach to real life scenarios
- The results showed reliable estimation of symptom severities, and suggest that the proposed approach can differentiate the patient’s symptoms with good precision during daily living, without imposing specific activities on patients
Orthopaedics
Whilst supporting the independent living needs of an ageing population, we observed that loneliness and anxiety were not the only concerns in the older adults’ lives. Many also experienced orthopaedic complications. This inspired our application of free-living, consumer-friendly wearable devices to diagnose symptoms and monitor treatment response.
Today, our data science team and research collaboration partners collect and expertly label the data of Orthopaedic patients, for the development and training of the Machine and Deep Learning algorithms. In parallel, our product development team built the end-to-end platform for both patients, clinicians and administrators.
Below are details covering the ongoing clinical research collaborations:
Singapore General Hospital (2018 – 2021)
- Evaluate the feasibility of using a patient activity tracking device for Total Knee Replacement patients including changes from pre-op to post-op, as well as to explore the association of analytics derived from the device with Patient Reported Outcome Measures (PROMS) commonly used in standard of care.
National University Hospital (2020 – 2021)
- Assessing functional recovery and augmenting PROMS using a Patient Activity Tracking Device for Total Knee Replacement patients.